Cows, along with many other farm animals, are susceptible to such an infectious disease as actinomycosis. It poses a great danger, since a person can also become infected with it. In this article, we will consider information about the symptoms, routes of infection, methods of prevention and treatment of actinomycosis.
What is actinomycosis
Actinomycosis is a chronic fungal infection of various organs and tissues of an animal and a person, which is characterized by the formation of granulomatous foci - actinomic. The disease affects all representatives of cattle (cattle), sheep, pigs, horses. It is observed in animals of various ages. Fixed all over the world. It can occur at any time of the year, but is most often diagnosed in the spring and winter.
The disease affects all representatives of cattle (cattle), sheep, pigs, horses. It is observed in animals of various ages. Fixed all over the world. It can occur at any time of the year, but is most often diagnosed in the spring and winter.
History reference
The actinomycosis pathogen was first isolated and described in 1877 as a microbe in the tissues of the jaw of a cow. Then the disease was called dixomycetus. In 1878, 2 cases of the disease identified in humans were described. They were registered in Germany. In the same year, German veterinarian Otto von Bollinger called the disease actinomycosis.
The causative agent was called a radiant fungus. Until 1940, it was believed that the causative agent of the infectious disease was identical with Actinomyces israelii. However, in the same year, D. Erickson proved that these are 2 separate organisms.
Did you know? The characteristic changes that the causative agent of actinomycosis provokes in the body of animals were discovered by scientists in the petrified jaws of a rhinoceros, dated to the Tertiary period.
Pathogen
The causative agent of actinomycosis is the gram-positive bacterium Actinomyces bovis, which is ranked as Actinomyces. It is susceptible to hot temperatures - it is destroyed in 5 minutes when heated to +70 ... + 80 ° C. Differs in resistance to drying. At low temperatures, lives for 1–2 years. Actinomyces bovis can be killed by exposure to a 3% formalin solution for 5–7 minutes.
Sources and routes of infection
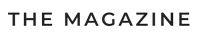
The causative agent enters the animal’s body through wounds in the oral mucosa when eating roughage (straw, cereal awns, mouse barley) or teething in calves, through damage to the skin, nipples of the mammary glands. Also, infection can occur anaerobically. The active growth of bacteria and the rapid development of the disease contributes to the presence in the body of purulent inflammation, trauma, and disturbances in the functioning of the immune system.
The active growth of bacteria and the rapid development of the disease contributes to the presence in the body of purulent inflammation, trauma, and disturbances in the functioning of the immune system.
The mechanism of the origin and development of the disease
After penetration into the body, the pathogen bacterium provokes the development of inflammation, in which granuloma forms. Most often, lesions are localized in the bones, tissues of the lower jaw, and lymph nodes. Subsequently, a tumor and fistula with yellowish purulent discharge containing gray Druze are formed. After in the purulent discharge is fixed blood and the remains of dead tissue.
Did you know? A cow can open and close its mouth about 30–40 thousand times a day. She makes most of these movements in order to chew gum.
Clinical signs
Clinical signs may be different, depending on in which part the pathogen is localized. A characteristic symptom is the presence of a dense tumor, which, as it develops, is opened, and pus flows from it.
With actinomycosis of the head, neck, jaw, tongue, the following symptoms are present:
- pain when touching an area with actinomycoma;
- pain when eating food;
- fever (rarely);
- leakage of pus from actinomic;
- change in the shape of the head;
- tooth loss;
- complication of breathing and swallowing as a result of the presence of actinomics in the respiratory tract, oral cavity, throat, tongue;
- exhaustion;
- increase and loss of language.
 If the pathogen settled in the intestine or abdominal cavity, then the following clinical symptoms develop:
If the pathogen settled in the intestine or abdominal cavity, then the following clinical symptoms develop:- temperature increase;
- pain in the peritoneum;
- vomiting
- diarrhea or constipation;
- partial intestinal obstruction.
Important! If tumors and fistulas are detected, treat the cow yourself. This can lead to undesirable consequences. At the first manifestations of the disease, you must seek veterinary care.
With actinomycosis, the udder is observed:
- necrosis of the skin;
- abscesses and fistulas in the mammary glands.
- tissue edema;
- depressed state;
- hyperthermia;
- redness or blueness of the skin at the site of inflammation.
Diagnostics
The disease is diagnosed during a veterinary examination and medical history. If it is required to exclude other diseases with similar symptoms (actinobacillosis, streptotrichosis, lymphangitis), then material is collected from actinomycoma for microscopy in laboratory conditions.
How to treat
When diagnosing actinomycosis, treatment of the disease should immediately begin. You need to start by placing the sick individuals in quarantine and processing the premises where they were kept with disinfectants.
Room disinfection
Disinfection is carried out with a 2-3% solution of caustic alkali or freshly slaked lime. The person who performs the disinfection must work in a special suit and observing personal safety measures.
Solution of iodine or potassium iodide
One treatment option is the intravenous administration of an iodine solution. It is prepared by mixing 1 g of iodine, 2 g of potassium iodide, 0.5 l of distilled water.
Antibiotics
Antibiotic therapy is also used against the pathogen. Possible introduction:
- Penicillin - 100-400 thousand units per tumor for 4-5 days;
- Oxytetracycline - 200 thousand units + 5-10 ml of saline to calves up to a year, 400 thousand units of adult individuals in healthy tissues surrounding the actinomy, for 10-14 days with simultaneous suction of pus from the tumor;
- Clindamycin;
- Erythromycin;
- a complex of antibiotic drugs with sulfonamides.
 In parallel with antibiotic therapy, autohemotherapy is carried out - blood transfusion from the jugular vein to the affected area.
In parallel with antibiotic therapy, autohemotherapy is carried out - blood transfusion from the jugular vein to the affected area.Surgical intervention
If conservative methods of treatment do not lead to an improvement in the condition of the cow and recovery, then surgery is performed - actinomycoms are opened, cleaned of pus and disinfected. After this, antibiotic therapy and the introduction of painkillers are performed.
After treatment, scars remain on the animal’s body. When the inflammatory process affects only the soft tissues, the cow can be completely cured. About whether the cows gain immunity against the disease after recovery is unknown. With damage to bones, joints, vital organs, the prognosis is poor.
Important! If treatment is not started on time, then the disease will go into a generalized form and affect the vital internal organs - liver, lungs, kidneys, brain, heart. Meat of such animals is forbidden to eat.
Prevention
In order to prevent this serious disease from entering the herd, it is necessary to adhere to some rules for keeping and feeding animals:
- Do not release cattle on pastures located in swampy lowlands.
- Before feeding coarse feeds, give it a heat treatment to soften and disinfect.
- Before putting straw into the feeder, it must be calcined.
- Regularly disinfect the room where the cows are kept and the equipment used to care for them.
- Periodically inspect animals for scratches and small wounds for timely treatment and treatment.
 Thus, actinomycosis is a serious infectious disease of cattle that affects animals, regardless of their age. It is characterized by the appearance on the body, most often in the area of the head and neck, of painful tumors that turn into fistulas with purulent contents. When the disease is detected in the early stages and the implementation of competent therapy, it lends itself to effective treatment.
Thus, actinomycosis is a serious infectious disease of cattle that affects animals, regardless of their age. It is characterized by the appearance on the body, most often in the area of the head and neck, of painful tumors that turn into fistulas with purulent contents. When the disease is detected in the early stages and the implementation of competent therapy, it lends itself to effective treatment.